×
The Standard e-Paper
Home To Bold Columnists
Courtesy
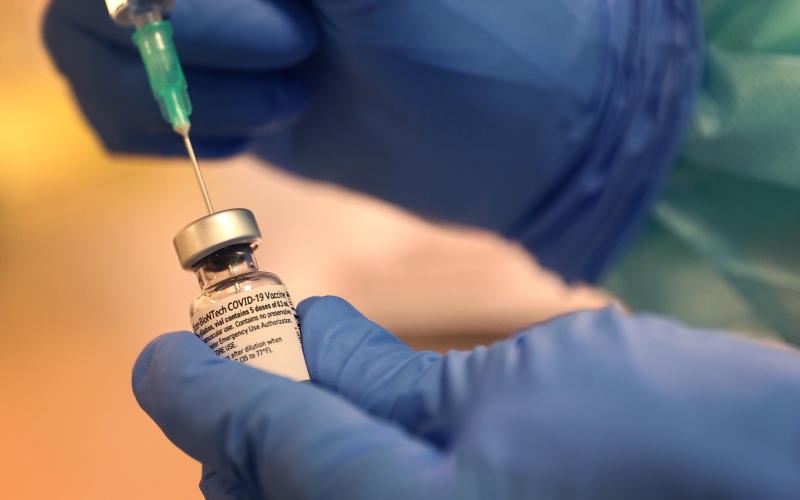
There are two misconceptions about Covid-19 testing and vaccine that we should all debunk. The first is that we can test our way out of the pandemic. Someone can test negative on Monday, feel sluggish on Tuesday, and go to an event on Wednesday, and unwittingly be spreading the virus. The test result reveals only whether the virus was detectable at the time of sampling.