×
The Standard e-Paper
Fearless, Trusted News
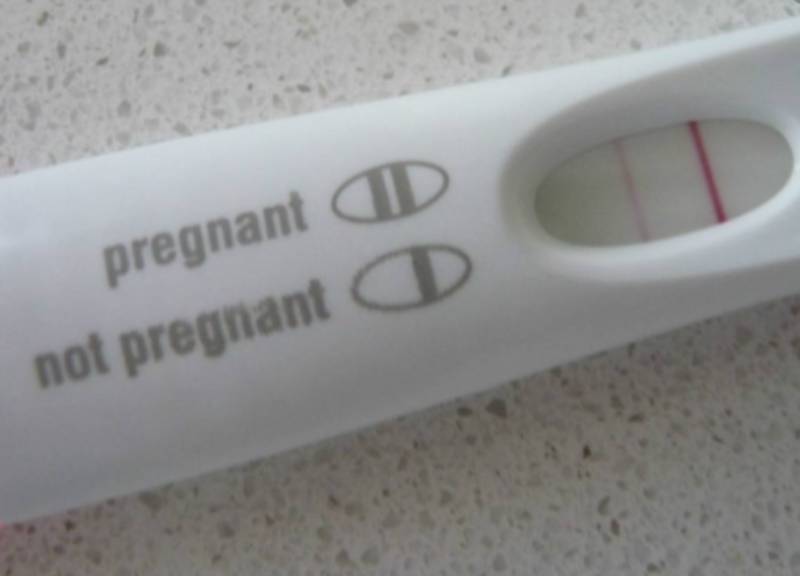
Like for all newlywed couples, life was supposed to follow a certain pattern for Mary when she got married. Get married, enjoy honey moon, get pregnant and enjoy family life. But that was not the case.