×
The Standard e-Paper
Fearless, Trusted News
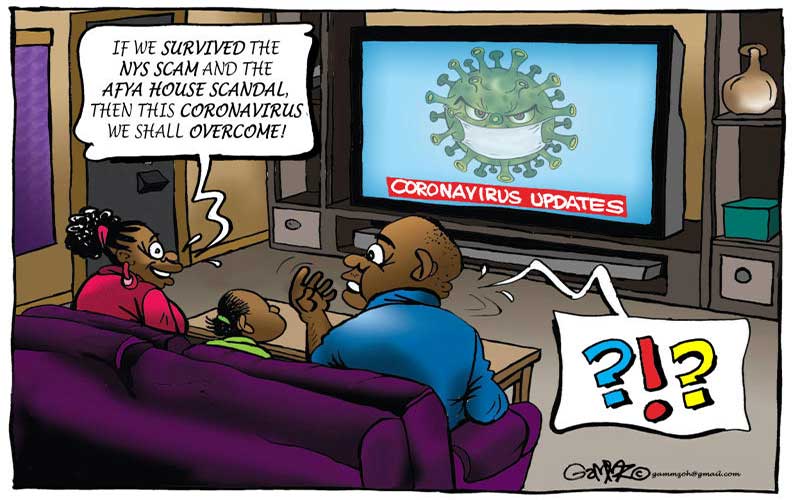
The Covid-19 coronavirus epidemic is not the first of its kind. A quick look at the history of the past provides lessons on what works or doesn’t, and how we ought to act to end this one.