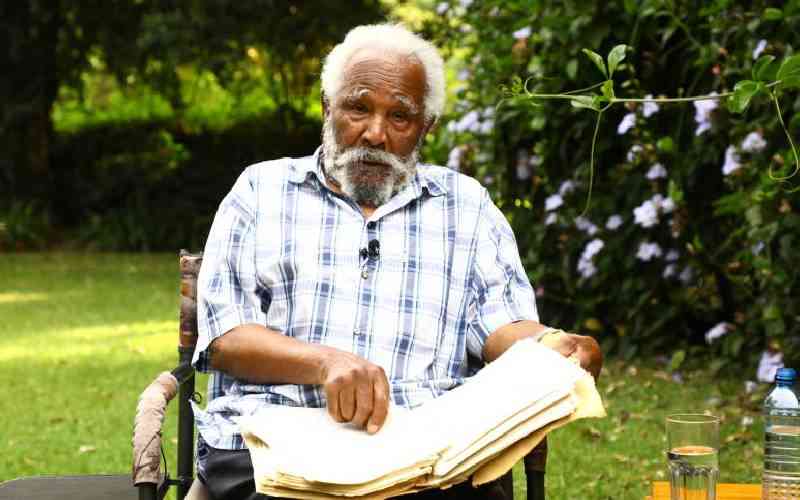
In the bustling corridors of Kenyatta National Hospital (KNH), Dr Reul Maina Kageni, an expert in Ear, Nose and Throat (ENT) disorders, has been witnessing a concerning trend.
A rare but potentially life-threatening condition known as Recurrent Respiratory Papillomatosis (RRP) is affecting an increasing number of patients, particularly children.
RRP is a viral disease characterised by the growth of cauliflower-like tumors in the respiratory tract, primarily affecting the voice box (larynx).
“It starts with hoarseness of voice, then progresses to difficulty in breathing,” Dr Maina explains. “It’s often mistaken for asthma, which can delay proper diagnosis and treatment.”
According to the doctor, the condition is caused by human papillomavirus (HPV) types 6 and 11, the same viruses responsible for genital warts.
The World Health Organization explains that RRP affects four out of every 100,000 children and 1-2 out of every 100,000 adults globally. However, these statistics may not accurately reflect the situation in Kenya.
The National Library of Medicine reports that RRP is more prevalent in developing countries, with several African nations being significantly affected.
- Pneumonia onslaught: Chest specialist's frontline battle
- For healthier lungs, avoid these 8 habits
- Unheard voices: Families silent war on respiratory papillomas
Keep Reading
While exact statistics for the continent are limited, countries like South Africa, Nigeria, and Kenya have reported higher incidence rates compared to global averages.
Dr Maina notes, “At KNH, we’ve treated approximately 350 patients with RRP, with children accounting for more than 300 of these cases. We believe this is just the tip of the iceberg. Many cases go undiagnosed, especially in rural areas where access to specialized care is limited.”
Studies have shown that children born to mothers under 20 years of age are at a higher risk of developing RRP. This is particularly concerning in Kenya, where teenage pregnancies remain a significant issue.
The Kenya Human Papillomavirus and Related Diseases Report highlights that the high prevalence of HPV in young women contributes to the risk of vertical transmission to infants during childbirth.
The patients Dr Maina sees are primarily children from low socio-economic backgrounds. This demographic trend aligns with global patterns, as studies have shown that RRP is more prevalent in populations with limited access to healthcare and lower vaccination rates against HPV. Diagnosing RRP requires specialized equipment and expertise. “We use laryngoscopy in the clinic for diagnosis,” Dr Maina explains.
“However, many patients come to us as emergency cases, unable to breathe, and are taken directly to the operating room.”
The mainstay of treatment is surgical removal of the papillomas. “On average, patients require surgery three times a year,” Dr Maina notes. This frequent need for intervention significantly impacts patients’ quality of life and poses a substantial financial burden on families and the healthcare system.
To improve care, Dr Maina and his team are advocating for advanced equipment like flexible laryngoscopes and intraoperative techniques such as microdebriders and lasers. These tools could enhance precision and potentially reduce the frequency of surgeries.
The link between RRP and HPV opens up possibilities for prevention and management, the doctor says.
The Gardasil vaccine, which protects against HPV types 6 and 11, has shown promise in reducing RRP recurrence rates.
“We aim to provide the vaccine to all patients,” he says. “Ideally, it should be affordable, if not free, to ensure widespread access.”
This approach aligns with recommendations from the National Institutes of Health (NIH) in the United States, which supports the use of HPV vaccines in RRP management.
However, implementing such strategies in Kenya faces challenges due to limited resources and competing health priorities.
Dr Maina and his colleagues have established a patient support group and are undertaking a national awareness program to educate healthcare providers and the public about the condition.
“Early detection leads to early intervention and good prognosis,” Dr Maina says. “We’re working to ensure that more healthcare providers can recognize the signs of RRP and refer patients appropriately.”
 The Standard Group Plc is a multi-media organization with investments in media platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national and international interest.
The Standard Group Plc is a multi-media organization with investments in media platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national and international interest.